
REG CHARITY: 513946 Based at Glenfield Hospital, Groby Road, Leicester, LE3 9QP
HEART LINK
HEART LINK ECMO
Heart Link are extremely proud to have funded the introduction of ECMO (Extra Corporeal Membrane Oxygenation) into Great Britain in 1989.
This is a modern invasive life-support technique which can be used in patients with extremely severe respiratory (lungs) and cardiac (heart) failure. The treatment is very expensive and labour intensive and, at this time, financial support from the NHS was out of the question.
Mr Richard Firmin, Paediatric Cardiac Surgeon at Groby Road Hospital, Leicester, approached Heart Link and convinced them to finance the introduction of an ECMO programme. Mr Firmin and Dr Sosnowski learned the technique on visiting the University of Michigan U.S.A which is where Prof. Bartlett, the father of ECMO, had developed the leading ECMO Centre.
Since November 1998 the Heart Link ECMO Centre (this is the official name of the ECMO programme) has treated numerous patients, not only babies but older children and adults. The Heart link ECMO Centre is now known world-wide as a very successful Unit.
ECMO is now financed by the NHS but there is still enormous input from Heart Link as we continue to help fund any ECMO research programme, finance medical and nursing staff who attend scientific meetings and teaching sessions, plus purchasing any new equipment needed to ensure that the highest and most modern standard of care is given to all those patients requiring ECMO treatment.

"ECMO" by Giles Peek
Consultant in Cardiothoracic Surgery & ECMO
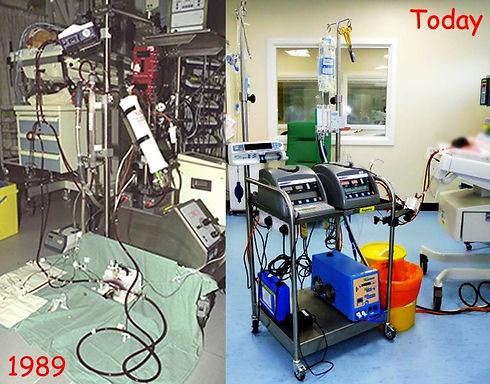
ECMO stands for Extracorporeal Membrane Oxygenation, what this means is the use of a machine, similar to the heart-lung machine used in the cardiac operating theatre, to take over the function of the lungs and/or heart for a period of days or weeks to give them a chance to recover. ECMO is only used when “normal” methods of intensive care are failing, it can be used in any situation where the lungs or heart are not working properly but have got a chance of recovery.
ECMO can therefore be used after a long, difficult and complex heart operation to support the function of the heart while it recovers. It could also be used in the case of someone who developed a severe lung infection with a virus such as the H1N1 virus (swine flu) to take over the function of the lungs to give the anti-viral drugs a chance to work.
In order to put a patient onto ECMO large pipes (cannulae) must be put into the blood vessels in the neck or groin, or sometimes directly into the heart itself, these allow blood to be drained away from the body to the ECMO machine where it is oxygenated before being pumped back into the patient. The tubing of the ECMO machine is made of plastic and this makes the blood try to clot, a drug called Heparin is used to prevent clotting, this means that patients are at risk of bleeding whilst they are on the ECMO machine. Patients who are on ECMO are very sick and the machine is very complex to look after so an extra nurse called an “ECMO Specialist” is always there to help look after patients whilst they are on ECMO. Often machines to replace the function of the kidneys or liver are also required, these can be connected to the ECMO machine to help the patient recover. Patients receive drugs to keep them pain free whilst they are on ECMO they also receive feeds either through a tube in the nose or intravenously. Some older patients who need to be on ECMO for a long time may be slowly woken up so that they can breathe for themselves.
The survival rates for patients treated with ECMO depend on what the underlying problem is. For instance for a patient whose heart is too weak to allow them to come off the heart-lung machine at the end of a difficult heart operation the expected survival with ECMO is about 50%, but if ECMO was not available in this situation no patients would survive. In the case of a new-born baby with lung failure ECMO can save one extra patient for every 3 patients treated, and for adults with lung failure one extra patient is saved for every 6 that are treated, compared to continued treatment with “normal” intensive care.
If you child or loved one needs to go onto ECMO it can be very frightening and confusing as they seem to be lost behind a row of machines, tubes and wires. But be reassured that the ECMO Team are working very hard to give your child the best chance of recovery and that they understand how scared and confused you are. Keep asking questions and you will soon understand how everything works and then you will be less scared and more able to help in the care of your child and regain a sense of control by contributing to their recovery.
We celebrate 25 years of the Heart Link ECMO Centre in 2014.

Web essentials
- UK Online Casinos Not On Gamstop
- UK Online Casinos Not On Gamstop
- Non Gamstop Casinos UK
- Betting Sites Not On Gamstop
- Non Gamstop Casinos UK
- Casino Not On Gamstop
- Non Gamstop Casino UK
- Non Gamstop Casino Sites UK
- Non Gamstop Casinos
- Casino Not On Gamstop
- Reputable Non Gamstop Casinos
- Casinos Not On Gamstop
- Casino Sites Not On Gamstop
- Non Gamstop Casinos
- Non Gamstop Casinos
- Best Non Gamstop Casinos
- Casinos Not On Gamstop
- Gambling Sites Not On Gamstop
- Top Betting Sites UK
- Casinos Not On Gamstop
- UK Online Casinos Not On Gamstop
- Betting Sites Not On Gamstop
- Casinos Not On Gamstop
- Non Gamstop Casino UK